Explainer Video
Pediatric Head Trauma Medical Decision Making Text
Medical Decision Making
Patient presenting with head trauma. Patient’s neurological exam was non-focal and unremarkable. Reviewing PECARN (Pediatric Head Injury/Trauma Algorithm): patient with no signs of altered mental status at this time, no overlying scalp hematoma, not severe mechanism of action, and no loss of consciousness greater thanŅ seconds putting him in the category of observation. Discussed with parent the risks and benefit of head imaging, and decided against Head CT. We observed the child for *** hours. Patient continued to act normally normally with no signs of neurologic changes. No episodes of vomiting. I considered SAH, SDH, Epidural Hematoma, IPH, and skull fracture in my differential but this appears unlikely considering the data gathered thus far. Do not believe there are signs of significant head trauma at this time. I do not believe that this is child abuse and that further investigation is necessary. Discussed warning signs of head injury that would prompt return to ED. Head trauma handout was provided. Return to emergency department urgently if new or worsening symptoms develop. Family expressed understanding of and agreement with plan and all questions answered.
Impression:
Head trauma
***
Plan
Discharge from ED
Tylenol for pain control.
Head trauma instructions provided in discharge instructions
Instructed Pt to monitor for neurologic symptoms, change in mental status, seizures, loss of consciousness, inability to eat. Instructed family to f/up w/ PCP in *** days or ETC should symptoms worsen or not improve.
Herpes Zoster / Shingles Full Note
History of Present Illness
Patient presenting for evaluation of rash. The rash is described as erythematous, vesicles. Onset of symptoms was 2 days ago. Rash is located on the torso. Associated symptoms include pain at area of rash Patient denies symptoms of shortness of breath, chest pain, oral/facial swelling, pruritus, fever Patient reports family members do not have similar rash. Symptomatic treatment prior to arrival includes lotions, Ibuprofen/Tylenol.
REVIEW OF SYSTEMS: All other systems reviewed and negative except as stated above in the HPI
Past medical history: None. No Medications or allergies.
Tobacco use: <1ppd
Alcohol Use: Yes
PHYSICAL EXAM:
Constitutional: No acute distress
HEENT: Head normocephalic and atraumatic. PERRL, EOMI. No scleral icterus or erythema. Pharynx moist without erythema or exudate.
CV: Regular rate and rhythm. No murmur. Peripheral pulses intact.
Respiratory: Lungs clear to auscultation bilaterally
Abdomen: Soft, non-tender, non-distended.
Back: No CVA or vertebral tenderness
Skin: Erythematous blistering vesicles in vary stages to ***
Extremities: Non-tender. No pedal edema.
Neuro: Oriented x3. No gross motor deficits
Medical Decision Making
presenting with ***. Presentation consistent with Herpes Zoster. No evidence of eye involvement. No evidence of infections including cellulitis, measles, rubella. Patient prescribed fungal shampoo. Supportive therapies discussed. Antiviral therapy prescribed. Discussed with patient that antiviral medications was associated with faster resolution of zoster-associated pain than acyclovir in patients > 50 years old (Ann Intern Med 1995 Jul 15;123(2):89). Follow up with primary physician in 7 days if symptoms continue. Discussed with patient that 10% zoster patients may have pain persisting at least 90 days despite medications (Mayo Clin Proc 2007 Nov;82(11):1341). Return to ED if high fever, significant spread , pain, or other concerns.
Impression:
Herpes Zoster
***
Plan:
Discharge from ED
Educated Pt on Dx of Herpes zoster, including typical resolution in 2-4wk
Prescribed acyclovir 800mg qid x10d OR valacyclovir 1000mg tid x7d, and instructed Pt to complete entire Ab course.
Prescribed hydrocodone-acetaminophen 5-500mg q6-8hr prn for pain
Advised OTC acetaminophen or ibuprofen as directed prn for pain
Prescribed lidocaine 2% jelly to apply topically q4hr prn.
Advised Pt to apply antibacterial salves or lotions topically to decrease the likelihood of bacterial infection of any blistering.
Advised Pt on supportive therapies, including application of warm compresses for pain control, loose/open shirts to decrease skin irritation, gently washing blisters w/ soap and H2O, refrain from opening any blisters, OTC analgesics, calamine lotion, and covering any ruptured lesions.
Advised Pt obtain live Zostavax shingles vaccine from PCP upon resolution of CC (unless allergy, immunocompromised [HIV/AIDS, CA, steroid Rx], pregnant, latent Tb).
Instructed Pt to monitor for signs of worsening pain or fever, neck stiffening, hearing loss, decreased cognition, worsening inflammation, or blistering w/ d/c; and directed Pt to f/up w/ PCP or ETC should Sx worsen or not improve. Pt verbally expressed understanding and all questions were addressed to Pt’s satisfaction.
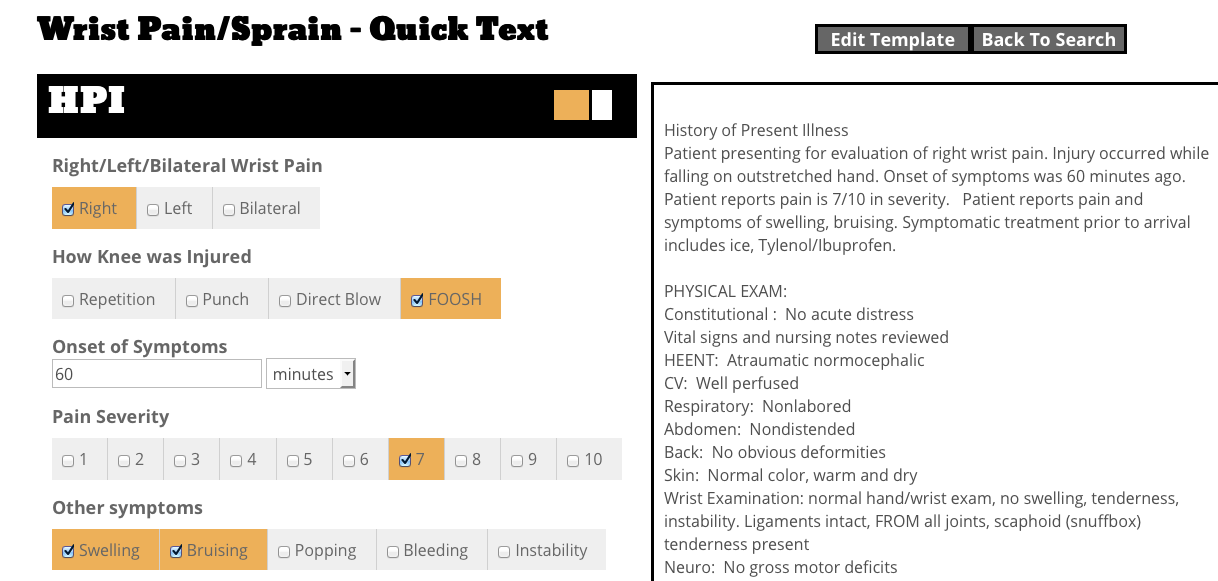
Carpal Tunnel Full Note
Patient presenting for evaluation of bilateral wrist pain. Injury occurred while at rest, no known injury. Onset of symptoms was 4 months ago. Patient reports pain is 5/10 in severity. Symptomatic treatment prior to arrival includes ice, heat, Tylenol/Ibuprofen.
All other systems reviewed and negative except as stated above in the HPI.
Past medical history: None. No Medications or allergies.
Tobacco use: None
Alcohol Use: No
PHYSICAL EXAM:
Constitutional : No acute distress
Vital signs and nursing notes reviewed
HEENT: Atraumatic normocephalic
CV: Well perfused
Respiratory: Nonlabored
Abdomen: Nondistended
Back: No obvious deformities
Skin: Normal color, warm and dry
Wrist Examination: normal hand/wrist exam, no swelling, tenderness, instability. Ligaments intact, FROM all joints, scaphoid (snuffbox) tenderness present
Neuro: Oriented x3, no gross motor deficits
Medical Decision Making
Patient presenting with ***. Presentation consistent with carpal tunnel syndrome. Radiographs were not ordered as there was no history of trauma. Patient with pain in the median nerve distribution. Phalen’s maneuver was *** (sensitivity of 51% to 91%, specificity of 33% to 88%). Tinel’s sign was *** (sensitivity of 95%, specificity of 56%). Provided wrist splint. Symptomatic treatment was discussed.. Patient may use ibuprofen/tylenol as needed for pain. Follow up with primary physician or orthopedic clinic if continued pain. Return to ED if pain uncontrolled, neurovascular change, or other concerns.
Impression:
Carpal Tunnel Syndrome
Hand Pain
***
Plan:
Discharge from ED
Wrist splint was fitted/applied and adjusted to the Pt. Discussed wearing, especially at night and monitor for improvement/resolution of numbness/tingling/pain.
Advised Pt on cold application to affected area forಔ-30 min q3-4hr for Ł -łd and then warm application to affected area for 20-30 min tid/qid until resolution of Sx.
Instructed Pt to take OTC acetaminophen or ibuprofen prn as directed.
Advised Pt refrain from or limit activities that exacerbate pain.
Instructed Pt to f/up w/ PCP should Sx worsen or not improve. Pt verbally expressed understanding and all questions were addressed to Pt’s satisfaction.